Looking into the lungs

Peter Lindholm studies breath-hold dive physiology.
Born and raised in Sweden, Peter Lindholm, M.D., Ph.D., enjoyed collecting tadpoles when he was little. Whether that activity sparked his interest in diving is uncertain, but his early interest in nature developed into an urge to become a scientist.
During medical school he joined a laboratory researching aviation, space and underwater physiology, where he developed a passion for breath-hold dive physiology, about which he wrote his doctoral thesis. He served on various committees on breath-hold diving, including the International Association for the Development of Apnea (AIDA, Association Internationale pour le Développement de l’Apnée).
As one of the physicians for the Swedish Sports Diving Federation (SSDF), which is part of the World Underwater Federation (CMAS, Confédération Mondiale des Activités Subaquatiques), he was involved in developing breath-hold dive protocols and training the first instructors of competitive breath-hold diving. After clinical training as a radiologist, Lindholm moved in 2019 to San Diego, California, where he leads a research group focused on dive physiology and dive medicine.
During medical school he joined a laboratory researching aviation, space and underwater physiology, where he developed a passion for breath-hold dive physiology, about which he wrote his doctoral thesis. He served on various committees on breath-hold diving, including the International Association for the Development of Apnea (AIDA, Association Internationale pour le Développement de l’Apnée).
As one of the physicians for the Swedish Sports Diving Federation (SSDF), which is part of the World Underwater Federation (CMAS, Confédération Mondiale des Activités Subaquatiques), he was involved in developing breath-hold dive protocols and training the first instructors of competitive breath-hold diving. After clinical training as a radiologist, Lindholm moved in 2019 to San Diego, California, where he leads a research group focused on dive physiology and dive medicine.
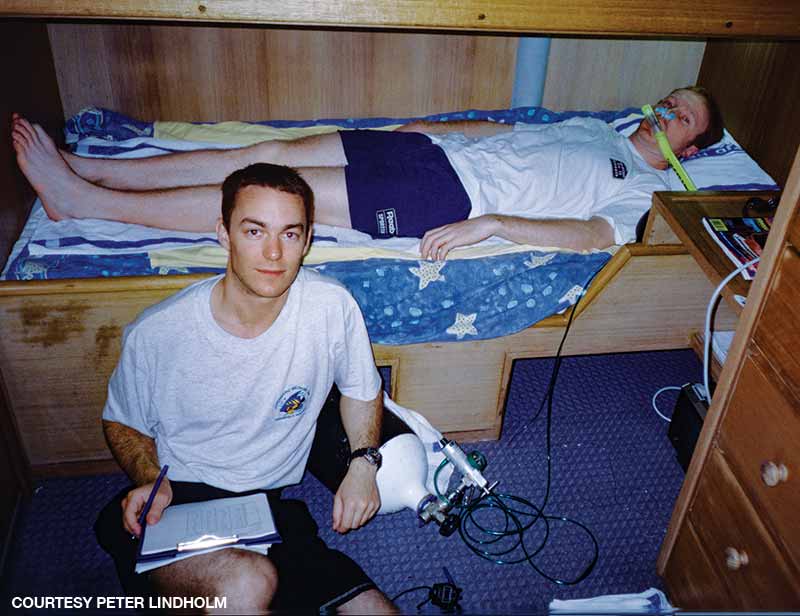 Lindholm uses a simple device for extending oxygen supply to a diver during field studies on a dive boat in the Coral Sea.
Lindholm uses a simple device for extending oxygen supply to a diver during field studies on a dive boat in the Coral Sea. Peter, tell us a bit about yourself. When did you become a diver?
I liked to snorkel when I was a kid, and my parents took me to the Maldives and the Red Sea when I was a teenager. I got my first dive certification when I was 16 years old. Everyone in Sweden had to join the military service for one year, and the military selected me for mine-clearance diving. We learned to dive to 200 feet (61 meters) on both open-circuit scuba and semiclosed rebreathers to search for things and blow them up. It took about nine months of training to become a mine-clearance diver, and then I was in operations for three months before my service ended.
What started your career in dive physiology?
Determined to become a researcher, I entered medical school at Karolinska Institutet after my military service and undergraduate studies in marine biology. After about two years I realized my interest in being a physician and switched my focus from animals in the sea to human divers. My dive background led me to Dag Linnarsson, M.D., Ph.D., who had experience in dive research and ran a lab where he was doing space research. He was a professor of baromedicine; the European Space Agency funded his work due to their interest in space-related cardiopulmonary research. That continuum of diving, high-altitude, aviation and space led to my doctoral thesis on hypoxia from breath holding.
After some literature review and talks with Dr. Linnarsson, I found that previous studies of breath-hold diving were not as thorough as I thought, so I started coming up with questions and ideas for answering those questions. Linnarsson encouraged my work, and we did some interesting projects together; that was the beginning of my thesis. I created my own M.D./Ph.D. program, and Karolinska was very supportive, although it extended my medical degree from the usual five and a half years to seven and a half years.
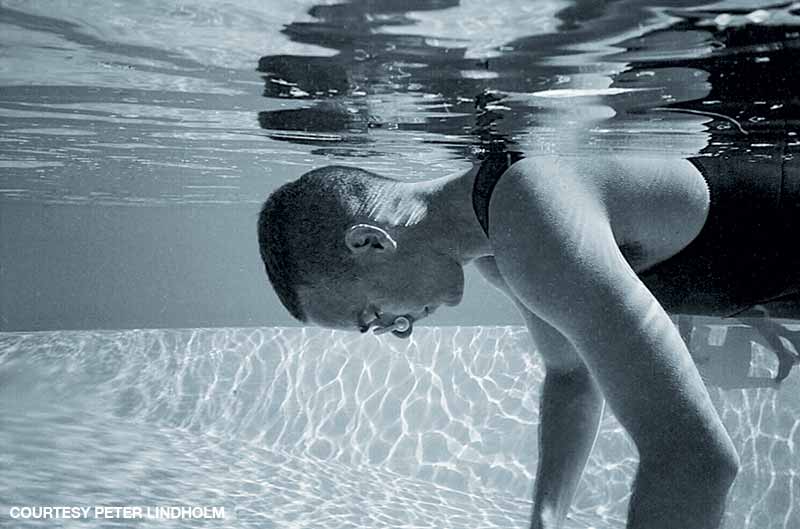 Lindholm practices static apnea in a pool in Sardinia during a freediving course in 2000.
Lindholm practices static apnea in a pool in Sardinia during a freediving course in 2000. Tell us more about your doctoral project.
When I started reading about breath-hold research, I realized that nobody had shown that a breath-holding human could conserve oxygen. There were, however, discussions about oxygen-conserving effects in diving mammals, which can dive for so long because they stop blood flow to their bodies and save oxygen for the brain.
There were some discussions about whether humans could save oxygen like that. I thought it would be interesting to investigate that question, so I decided to study it during exercise instead of resting conditions. When a freediver is resting, not much blood is going to the muscles anyway, and most of the oxygen consumption already occurs in the brain, so that wouldn’t be a useful model.
A second necessary step was to eliminate the diving response from the equation without affecting oxygen storage. We did that by having participants use a bag to rebreathe their exhaled air, which will trick the body into thinking that you’re breathing normally, but you don’t get any new oxygen.
In the experiment with exercising human subjects, we showed that working muscles’ basic vascular constriction was just enough to be significant, which means we proved a temporary oxygen-conserving effect. Some important parameters we measured were vasoconstriction, heart rate and cardiac output. The amount of blood the heart pumps out is the most critical variable, although it’s harder to measure than the heart rate and oxygen levels in the lungs and blood.
Did you stay involved with the military during or after your studies?
In Sweden, the military can call you back at any time. After you pass the surgery exam in medical school, the military can repurpose you as a surgeon in the event of war. Upon getting my Swedish medical license, I was eligible to take the military dive physician course, which lasts several weeks and includes field practicals in dive medicine and submarine escape. It was a great experience to return after more than 10 years. I occasionally served a couple of weeks as a dive physician in my old unit in the Swedish navy.
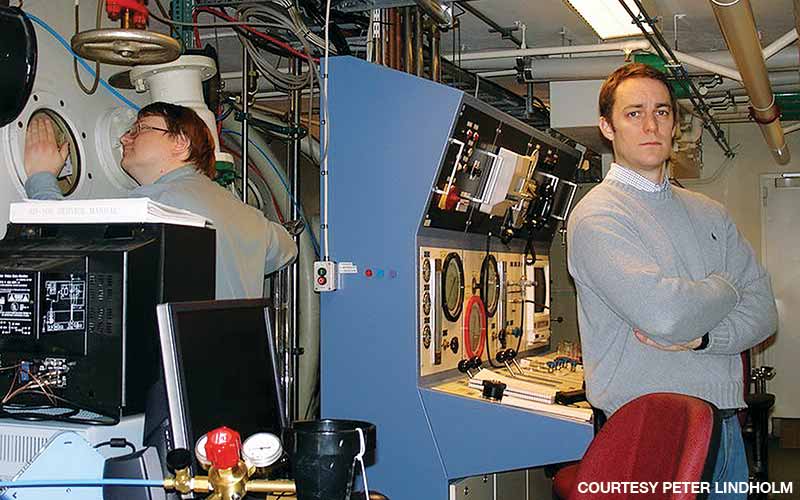 Lindholm oversees experiments in the high-altitude chamber at Karolinska. The chamber can range in pressure from depths of 500 feet to altitudes of 100,000 feet.
Lindholm oversees experiments in the high-altitude chamber at Karolinska. The chamber can range in pressure from depths of 500 feet to altitudes of 100,000 feet. What brought you to the U.S.?
I did postdoctoral work at the University at Buffalo, where my assignment helped me gain more research experience. My supervisor there was Claes Lundgren, M.D., Ph.D. I also did some experiments with Massimo Ferrigno, M.D., at Harvard. They are exceptional breath-hold dive researchers. I returned to Sweden after that postdoctoral assignment.
My medical training was as a radiologist; I did radiology research and then became director of thoracic radiology at Karolinska. Having kids didn’t leave time for me to do dive research for about five years. When my wife got a postdoctoral position at Stanford University, I took a sabbatical and went with her. I got a visiting professorship at Stanford, which got me back to doing research. I didn’t have any clinical obligations and picked up some of my old ideas for breath-hold dive research. Because my interest is thoracic radiology, I researched pulmonary edema — what some breath-hold divers call “the squeeze.” I had published a paper on the squeeze in 2008 from research we did with people diving in a tank with empty lungs, so I resumed that topic in 2017.
My wife and I wanted to stay in California. When the University of California San Diego advertised a position in hyperbaric and dive medicine, I applied for it and got it.

Lindholm experiences 22 seconds of weightlessness after finishing zero-gravity parabolic flight experiments to study pulmonary physiology.
What are your current breath-hold research projects?
I am focusing on squeeze effects in which the lungs suffer compression at depth and problems such as immersion pulmonary edema and hemoptysis from bleeding in the lungs. I’m also studying swimming-induced pulmonary edema (SIPE). We have a large group to study in San Diego since some Navy SEAL candidates suffer SIPE when trying to pass Basic Underwater Demolition/SEAL training.
Pandemic aside, do you still breath-hold dive?
I did some freediving in Hawaii last New Year’s, but I’m more of a snorkeler now. I don’t do competitive freediving. Back around 2000, when I was seriously practicing for it, I could freedive to 40 meters and breath hold for five minutes.
If you wanted to get back to a five-minute breath hold, how long would it take you to train for that?
I’m not sure — maybe two weeks?
Note: Two weeks after the initial interview, Lindholm reported that he had felt obliged to test his statement. Having not done any breath-hold training for the past decade, he was able to return to 4 minutes and 47 seconds in dry static apnea.
Collaborations and Current Research Focus
Lindholm has secured a collaborative grant from the Navy to build a database of old audio Doppler files. Doppler ultrasound has been used for decades to record audio signals of bubbles in the bloodstream after a dive, so there is an enormous amount of data from experiments by the Navy, universities and DAN. The plan is to collect the files in a gigantic database and use artificial intelligence to automate grading them so researchers can use the
data to better understand decompression stress.
Lindholm is also collaborating on the DAN COVID-19 study as an expert consultant on lung imaging and has received funding for a project that examines decompression stress in breath-hold divers. Researchers have long ignored this topic, as the general perception is that decompression sickness cannot occur when diving without compressed gas.
Explore More
Watch Peter Lindholm discuss the physiology of breath-hold diving in this video.
© Alert Diver — Q2 2021
Posted in Alert Diver Summer Editions, Dive Fitness, Dive Safety FAQ
Posted in Breath Hold Diving, Breath hold, Peter Lindholm, Physiology, Apnea, Pure Apnea
Posted in Breath Hold Diving, Breath hold, Peter Lindholm, Physiology, Apnea, Pure Apnea
Categories
2025
2024
February
March
April
May
October
My name is Rosanne… DAN was there for me?My name is Pam… DAN was there for me?My name is Nadia… DAN was there for me?My name is Morgan… DAN was there for me?My name is Mark… DAN was there for me?My name is Julika… DAN was there for me?My name is James Lewis… DAN was there for me?My name is Jack… DAN was there for me?My name is Mrs. Du Toit… DAN was there for me?My name is Sean… DAN was there for me?My name is Clayton… DAN was there for me?My name is Claire… DAN was there for me?My name is Lauren… DAN was there for me?My name is Amos… DAN was there for me?My name is Kelly… DAN was there for me?Get to Know DAN Instructor: Mauro JijeGet to know DAN Instructor: Sinda da GraçaGet to know DAN Instructor: JP BarnardGet to know DAN instructor: Gregory DriesselGet to know DAN instructor Trainer: Christo van JaarsveldGet to Know DAN Instructor: Beto Vambiane
November
Get to know DAN Instructor: Dylan BowlesGet to know DAN instructor: Ryan CapazorioGet to know DAN Instructor: Tyrone LubbeGet to know DAN Instructor: Caitlyn MonahanScience Saves SharksSafety AngelsDiving Anilao with Adam SokolskiUnderstanding Dive Equipment RegulationsDiving With A PFOUnderwater NavigationFinding My PassionDiving Deep with DSLRDebunking Freediving MythsImmersion Pulmonary OedemaSwimmer's EarMEMBER PROFILE: RAY DALIOAdventure Auntie: Yvette OosthuizenClean Our OceansWhat to Look for in a Dive Boat
2023
January
March
Terrific Freedive ModeKaboom!....The Big Oxygen Safety IssueScuba Nudi ClothingThe Benefits of Being BaldDive into Freedive InstructionCape Marine Research and Diver DevelopmentThe Inhaca Ocean Alliance.“LIGHTS, Film, Action!”Demo DiversSpecial Forces DiverWhat Dive Computers Don\'t Know | PART 2Toughing It Out Is Dangerous
April
July
